“If I do this, will it be considered suicide?” This question was posed to me 34 years ago while I was the chaplain at the Fairfax Nursing Center in the D.C. suburbs of Virginia. It came to mind as I read a recent article in The New York Times.
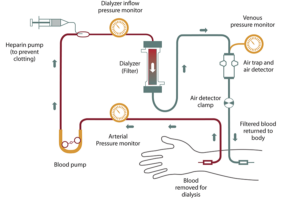
Source: National Inst. of Health
“Dialysis May Prolong Life for Older Patients. But Not by Much,” by Paula Span unpacks the results of a recent medical research study published in the Annals of Internal Medicine. The researchers compared the length of life and quality of life of two groups of elderly patients with advanced kidney disease. One group started dialysis to manage their disease, and another group declined dialysis.
But the group that declined dialysis didn’t just DO NOTHING. Here’s how the NY Times article put it:
“The alternative to dialysis goes by various names — medical management, conservative kidney management, supportive kidney care. In this scenario, nephrologists monitor their patients’ health, educating them about behavioral approaches, prescribing anti-nausea drugs like Zofran and diuretics like Lasix to reduce fluid retention, and adjusting their doses as needed.”
I contacted my nephrologist friend, Dr. Alvin Moss, at the West Virginia University School of Medicine. He has long been an advocate for treating kidney failure in elderly patients without resorting to dialysis. He said his patients like to call this approach, “active medical care without dialysis!”
I wrote about this topic in a blog post three years ago. Also, if you want to watch a humorous spin on the very serious subject of the for-profit dialysis business go to Dialysis: Last Week Tonight with John Oliver.
Longer life with worse quality of life
It is true that those on dialysis lived longer, on average, about 25 months, where the group receiving active medical care without dialysis lived about 23 months. But the quality of life for the dialysis patients was worse.
The dialysis group spent about two weeks less at home (in a hospital or nursing home) than those getting supportive care. Almost all the dialysis patients had to travel to a center three times a week to be hooked up to a machine for several hours each visit. Yes, they lived 2 months longer, but with greater burdens.

Photo by Harry cao on Unsplash
Here is one patient’s approach to the dialysis decision from the NY Times article:
“Even before Georgia Outlaw met her new nephrologist, she had made her decision: Although her kidneys were failing, she didn’t want to begin dialysis.
“Ms. Outlaw, 77, a retired social worker and pastor in Williamston, N.C., knew many relatives and friends with advanced kidney disease. She watched them travel to dialysis centers three times a week, month after month, to spend hours having waste and excess fluids flushed from their blood.
“‘They’d come home weak and tired and go to bed,’ she said. ‘It’s a day until they feel back to normal, and then it’s time to go back to dialysis again. I didn’t want that regimen.’
“She told her doctors, ‘I’m not going to spend my days bound to some procedure that’s not going to extend my life or help me in any way.’”
Nursing home patient stopped dialysis
What happened to the patient worried about suicide?
That patient who asked me about suicide? You guessed it. He was on dialysis and had had enough. He wanted to stop the treatment and die peacefully in the nursing home. He was also a very devout Catholic and wanted assurance that stopping dialysis was not suicide.
“Of course not,” I told him. “You will be dying from kidney failure. It will be a very natural death.” He got that peaceful death he wanted.
__________________
Author Chaplain Hank Dunn, MDiv, has sold over 4 million copies of his books Hard Choices for Loving People and Light in the Shadows (also available on Amazon).

