“They” say men of a certain age are concerned about performance. Last week, while hiking the Big Schloss in 97-degree heat, this crossed my mind as I asked myself, “Can I do this again?”

Sundown on the Big Schloss
My bladder cancer surgery in May canceled a long-planned trip to see my adult children and my teenaged grands. I missed my grandson’s high school graduation and my youngest daughter’s engagement party. Unfortunately, those events can never be duplicated, but I hoped this trip would compensate for lost time.
In the last two weeks, I made the delayed trip to the D.C. suburbs of Virginia, my home from 1978 to 2017. Just like when I traveled the country speaking, once I had a destination, I looked into how I could spend some time in the great outdoors — preferably including wilderness travel.
“Grandpa, how did you get into hiking and backpacking?”

Hank & grands on 2016 hike
I used to take my three grands on overnight backpacking or car camping trips. They have slept with bugs, spiders, mice, snakes, and other inconveniences and even encountered a bear. They were always good sports at the time but have declined invitations to repeat any of these adventures in recent years.
So now on my trips to visit family, I try to plan a meal with just my grandkids and me to get some quality time and have an “ask-me-anything” session. This time, we went to Chili’s right after I returned from an overnight in the woods.

Out to eat with the grands.
Over hamburgers and fries, my grandson asked, “Grandpa, how did you get into hiking and backpacking?” I thought back. It was actually a chance reading of a Redbook magazine article. In 1971, while I was in seminary, I had taken their grandmother to the doctor’s office. This was back before we could occupy ourselves with phones when waiting rooms were piled with old magazines.
Hank, left, and Charles. First backpack trip, 1974
The Redbook article was about a five-day backpacking trip into the backcountry of Yellowstone National Park. The writer was in one of the most visited parks in the country, and they never encountered another human during the whole trip. I said to myself, “I want that.”
Thus, my love of wilderness camping was born in the waiting room of a doctor’s office. It took a while, but my first overnight carry-everything-on-my-back-away-from-roads-and-the-grid trip was on March 1, 1974.
My most recent trip was July 16, 2024.
“Can I do this again?”
As I mentioned, while planning this last trip, I wanted to add a night in the woods amid visits to family and friends. The Big Schloss was an ideal choice, less than a two-hour drive from Northern Virginia. “Schloss” is the German word for castle, and the rocks on the summit indeed look like a castle from below.

No tent, just a tarp, priceless
It is only a two-mile hike and 850 feet of elevation gain to the campsite near the summit. I have probably slept on this mountain thirty times since my first trip there in 1980, when I introduced my then-six-year-old son to backpacking.
While I was a hospice chaplain, I even figured out a way to hike the Big Schloss on a workday in the summer. Because of the long daylight hours, I could leave my last patient at 5 PM, arrive at the trailhead by 7, and set camp by sundown around 9. Then, I would wake at first light in the morning, pack up, drive home, shower, and be at work by 10.
I invited my future son-in-law, Will, to join me on last week’s trip. Though he never backpacked or spent much time in the woods, he said yes. So, we left the trailhead and headed up the mountain together. The first half mile is all uphill, about 600 feet. Next, an up-and-down walk along the ridge that forms the Virginia and West Virginia border. Finally, the last quarter of a mile is all uphill, about 200 feet.
The 97-degree heat, the incline, and the 35 pounds on my back all made this a brutal hike. We made it, but to be honest, it took me several hours to recover. While recovering, we set up our tarps to sleep under and cooked dinner. After dinner we had an enjoyable campfire with some “deep thoughts” conversation.
Who was I trying to convince, “Yes, I CAN do this again”? Will, who is a strong twentysomething? You, who are reading this blog? Myself? The Universe? All the above?
A surprise test

Hank & Will, on the way down from the Big Schloss
It is not just my bladder cancer but my age that thrusts this question upon me. I will NOT be able to do this forever. Stroke, heart failure, or cancer could disable or kill me. Did I just take my last backpacking trip? Perhaps.
I don’t want to make this sound morbid. Au contraire, this is a moment to be thankful for all those wilderness outings, particularly for this most recent one.
Before returning to Arlington, Will and I stopped for breakfast at a diner on Route 11 in Woodstock, Virginia. I congratulated him over coffee, eggs, sausage, biscuits, and grits. “Will, you passed the test. You can marry my daughter.”
Surprised, he said, “TEST? I didn’t know this backpacking trip was a test!”
Oh yeah. It was. For both of us.
[NOTE: I did a short video while backpacking, talking all this. CLICK HERE]
__________________
Author Chaplain Hank Dunn, MDiv, has sold over 4 million copies of his books Hard Choices for Loving People and Light in the Shadows (also available on Amazon).
Follow Hank: LinkedIn | Instagram | Facebook | YouTube


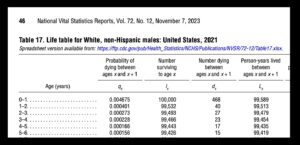 I’ve already had my last colonoscopy a couple of years ago. Even before my cancer, I had accepted the guidelines that there was no need to screen for something that would not kill me before my
I’ve already had my last colonoscopy a couple of years ago. Even before my cancer, I had accepted the guidelines that there was no need to screen for something that would not kill me before my  In the immediate future, I will take a road trip to visit my three children and four grands. I have made this trek two or three times a year for several years. I love driving long distances; this one is over 3,000 miles round trip. I will listen to books and podcasts, see my people, and visit friends, some of them going back to the 1970s. I will also visit places that will bring back so many memories. I want to get this DONE.
In the immediate future, I will take a road trip to visit my three children and four grands. I have made this trek two or three times a year for several years. I love driving long distances; this one is over 3,000 miles round trip. I will listen to books and podcasts, see my people, and visit friends, some of them going back to the 1970s. I will also visit places that will bring back so many memories. I want to get this DONE.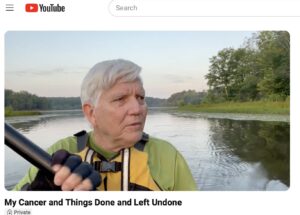



 While waiting for the daughter’s arrival, the ER doc asked me, “What is his code status?” I told him.
While waiting for the daughter’s arrival, the ER doc asked me, “What is his code status?” I told him.

 This story about this patient and his daughter came to mind as I listened to a recent GeriPal podcast,
This story about this patient and his daughter came to mind as I listened to a recent GeriPal podcast, 


 I am guessing if, during that last phone call, Favre asked, “Do you regret getting the chemo?” Keith might have responded, “Not at all.” Perhaps it bought him some time. Maybe, earlier in the treatment, he did not think it was causing “more damage… than the cancer.”
I am guessing if, during that last phone call, Favre asked, “Do you regret getting the chemo?” Keith might have responded, “Not at all.” Perhaps it bought him some time. Maybe, earlier in the treatment, he did not think it was causing “more damage… than the cancer.”




 I read a recent JAMA Online article titled “
I read a recent JAMA Online article titled “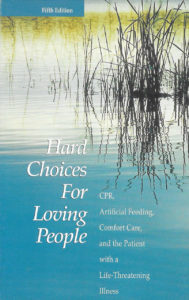 Changing “What does the patient WANT?” to “What does the patient THINK…”
Changing “What does the patient WANT?” to “What does the patient THINK…”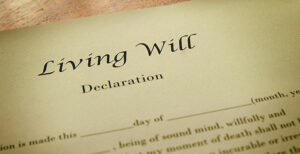 Soon after I became a part-time nursing home chaplain in 1983, our administration formed an ethics committee. Virginia had just passed a “Natural Death Act,” which gave patients a right in the code to refuse treatment and provided a form (e.g., “living will”) to express their treatment preferences.
Soon after I became a part-time nursing home chaplain in 1983, our administration formed an ethics committee. Virginia had just passed a “Natural Death Act,” which gave patients a right in the code to refuse treatment and provided a form (e.g., “living will”) to express their treatment preferences.