I’ve never been one for a “bucket list.” You know — the one with skydiving and climbing Mt. Kilimanjaro on it. Never thought of those things.
But, I do think of “things to do”. They come to mind, and I say to myself, “I really need to do this before I get so disabled or demented that I can’t finish them.”
For what it’s worth, here are some of mine.
- Update our wills. It has been years since we last did this. We’ve moved to a new state—TWICE—Florida and now Mississippi. We’ve launched our daughter out from under our roof (never out of our hearts). There have been many other changes in our situation that make this update necessary.
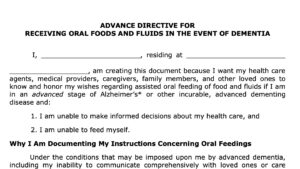
 Update our advance directives. I wrote a blog recently about Voluntary Stopping Eating and Drinking (VSED) by advance directive. I want to add instructions on when to stop hand feeding me if I have advanced dementia. Putting this in writing can be very easy to do with samples I linked in the blog. Then, of course, we need to have two friends over to witness my signature.
Update our advance directives. I wrote a blog recently about Voluntary Stopping Eating and Drinking (VSED) by advance directive. I want to add instructions on when to stop hand feeding me if I have advanced dementia. Putting this in writing can be very easy to do with samples I linked in the blog. Then, of course, we need to have two friends over to witness my signature.- Review beneficiaries on retirement accounts. This one we have done recently but I’ll check again just to make sure they say what I want them to say.
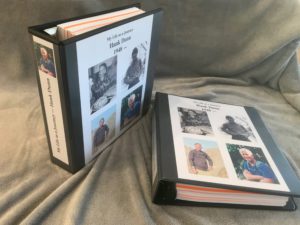 Continue to gather my “memoir” for my kids and grands. I wrote a blog around my birthday in 2021 about “keeping your regret list short.” It was kind of a “bucket list” thingy and I mentioned the notebooks I had gathered for my children and their children. Well, I have written more since then, so I need to keep on gathering. I also print my favorite quotable-quotes file (36 pages long). Interestingly, I found among dad’s papers, a notebook he kept of his favorite quotes, probably dating from the 1950s. When I started my own compilation of quotes, I had no idea he had done the same.
Continue to gather my “memoir” for my kids and grands. I wrote a blog around my birthday in 2021 about “keeping your regret list short.” It was kind of a “bucket list” thingy and I mentioned the notebooks I had gathered for my children and their children. Well, I have written more since then, so I need to keep on gathering. I also print my favorite quotable-quotes file (36 pages long). Interestingly, I found among dad’s papers, a notebook he kept of his favorite quotes, probably dating from the 1950s. When I started my own compilation of quotes, I had no idea he had done the same.- Finish my “spiritual autobiography.” I am in a small group at church, and we all are writing a spiritual autobiography to share with the group. I have a draft and will continue of refine it. I want to get it in a form suitable to give a copy to each child and grandchild. My spiritual life is so central to who I am, and I want to let those who love me know what is bubbling up inside. I don’t think they have any idea.
These are all doable items — and so important to me.
What about you? What’s bubbling inside on your important “things-to-do” list.
________________________________________
Chaplain Hank Dunn is the author of Hard Choices for Loving People: CPR, Feeding Tubes, Palliative Care, Comfort Measures and the Patient with a Serious Illness and Light in the Shadows. Together they have sold over 4 million copies. You can purchase his books at hankdunn.com or on Amazon.


 Several years ago, I spoke at the Centra Hospital in Lynchburg, Virginia. There were about 50 people in the room, including members of the clergy, physicians, nurses, social workers, and just plain folks. I divided my presentation, the first half devoted to helping patients and families make end-of-life decisions, and the second half to the emotional and spiritual issues at the end of life.
Several years ago, I spoke at the Centra Hospital in Lynchburg, Virginia. There were about 50 people in the room, including members of the clergy, physicians, nurses, social workers, and just plain folks. I divided my presentation, the first half devoted to helping patients and families make end-of-life decisions, and the second half to the emotional and spiritual issues at the end of life. About six months after the patient died, the lady visited her friend. The now-widow said, “I made a mistake. I made the wrong decision. I should have left the tube out and let him die sooner.”
About six months after the patient died, the lady visited her friend. The now-widow said, “I made a mistake. I made the wrong decision. I should have left the tube out and let him die sooner.”