Former President Jimmy Carter continues to teach us how to age with grace and meaning. I blogged previously about his going on hospice back in February. Now, six months later, he is still alive and receiving hospice care at home.
Three lessons we can take away from this phase in his life:
-
Hospice care can continue longer than six months
 To qualify for hospice under the Medicare benefit, a physician has to say, “This patient has, at most, six months to live if the disease runs its normal course.” What happens if the prognosis is wrong and the patient is still alive after six months?
To qualify for hospice under the Medicare benefit, a physician has to say, “This patient has, at most, six months to live if the disease runs its normal course.” What happens if the prognosis is wrong and the patient is still alive after six months?
Note the caveat, “if the disease runs its normal course.” Some patients do live longer than is expected. In these cases, the hospice can re-certify that the patient still appears to have six months or less to live.
Some diagnoses are very difficult to guestimate the number of months a patient may have left. For instance, cancers are easier to give a prognosis than dementias. Doctors just do the best they can.
50% of hospice patients are on hospice care for 18 days or less.* 25% receive care for just five days or less. But there are outliers on the long end, with 10% on service for more than nine months. So, Jimmy Carter’s six months does happen more often than you might think.
-
Hospice care is primarily delivered in the place of residence

Carter home in Plains, Georgia. Photo: Library of Congress
Many people think hospice is a place you go to die. Not true. Hospice is a concept of care. 98% of hospice care is delivered in the patient’s residence, whether that is a private home, an assisted living facility, or a nursing home.
A recent Washington Post article gave a window into life in the Carter home now.
“Jimmy Carter is often out of bed first, waiting in his recliner for his wife to emerge. ‘Rosalynn comes in the room and makes a beeline for this chair and bends over and kisses him,’ said Jill Stuckey, a close friend. They spend many hours sitting side by side.”
-
Families usually provide most of the caregiving for hospice patients
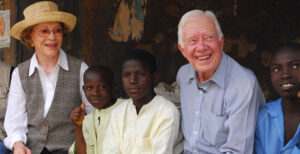
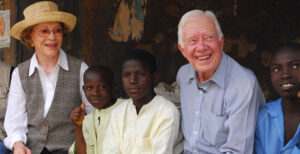
Place: Nasarawa North, Nigeria; Feb. 15, 2007; Credit: The Carter Center
Many families are surprised that hospice does NOT routinely provide round-the-clock care. The family must provide the bulk of the care. Only 1% of hospice dollars go to what is known as “continuous care,” meaning round-the-clock.
Of course, the Carters have the resources to get the best care at home. They have other perks too. The Secret Service gave the couple a ride to watch the Fourth of July fireworks in their hometown.
Interestingly, Rosalyn Carter has had a passion for providing support for family caregivers. When The Carter Center announced that Mrs. Carter was diagnosed with dementia, they commented, “As the founder of the Rosalynn Carter Institute for Caregivers, Mrs. Carter often noted that there are only four kinds of people in this world: those who have been caregivers; those who are currently caregivers, those who will be caregivers, and those who will need caregivers.”
Thank you for your service
The Post asked people who knew them what makes the Carters keep going. “Gerald Rafshoon, who was Carter’s White House spokesman, and others believe a key reason the Carters keep going is that neither wants to leave the other.”
The Carters have lived a life of service and continue to provide an example of how to approach the last days. Thank you, Jimmy and Rosalyn!
_______________
*Statistics in this blog came from the National Hospice and Palliative Care Organization’s “Facts and Figures, 2022 Edition.”
________________________
Chaplain Hank Dunn is the author of Hard Choices for Loving People: CPR, Feeding Tubes, Palliative Care, Comfort Measures and the Patient with a Serious Illness and Light in the Shadows. Together they have sold over 4 million copies. You can purchase his books at hankdunn.com or on Amazon.



 To qualify for hospice under the Medicare benefit, a physician has to say, “This patient has, at most, six months to live if the disease runs its normal course.” What happens if the prognosis is wrong and the patient is still alive after six months?
To qualify for hospice under the Medicare benefit, a physician has to say, “This patient has, at most, six months to live if the disease runs its normal course.” What happens if the prognosis is wrong and the patient is still alive after six months?






 The patient had left verbal and written instructions that she did not want to have life-saving treatments when she was dying. A “No CPR” order was on her chart. Knowing her daughter’s feelings, the old lady chose her son as her power of attorney. She conspicuously omitted any mention of her daughter in the document.
The patient had left verbal and written instructions that she did not want to have life-saving treatments when she was dying. A “No CPR” order was on her chart. Knowing her daughter’s feelings, the old lady chose her son as her power of attorney. She conspicuously omitted any mention of her daughter in the document.


