“I quit chemo…and it probably did more damage to me than the cancer did….” This was Toby Keith’s feelings about chemotherapy, according to his friend Brett Favre.
So, is the takeaway to never do chemo? Absolutely NOT.

Photo by Hiroshi Tsubono on Unsplash
Country singer Toby Keith was diagnosed with stomach cancer in 2021. About six months later, he announced to his fans on social media that he was receiving chemotherapy, radiation, and surgery.
“So far, so good,” Mr. Keith wrote in a June 2022 statement on multiple social media platforms. “I need time to breathe, recover, and relax. I am looking forward to spending this time with my family. But I will see the fans sooner than later. I can’t wait.”

Keith’s last concert in Las Vegas, (TobyKeith.com)
Indeed, he got back out there and played a series of shows in Las Vegas less than two months prior to his death a few weeks ago. In an interview right before he died, he said, “Cancer is a roller coaster. You just sit here and wait on it to go away — it may not ever go away.”
“[Keith] handled it with grace and faith and family and stood up to the cancer as good as you can,” said the former Green Bay Packers quarterback. “[But] I think in the end he was just tired,” Favre added.
We can hardly base treatment decisions on one man’s experience. Mr. Keith, diagnosed at age 60, made his decision based on the type of cancer he had and his own unique goals of care at that stage in the disease.
 I am guessing if, during that last phone call, Favre asked, “Do you regret getting the chemo?” Keith might have responded, “Not at all.” Perhaps it bought him some time. Maybe, earlier in the treatment, he did not think it was causing “more damage… than the cancer.”
I am guessing if, during that last phone call, Favre asked, “Do you regret getting the chemo?” Keith might have responded, “Not at all.” Perhaps it bought him some time. Maybe, earlier in the treatment, he did not think it was causing “more damage… than the cancer.”
In my years as a hospice chaplain, I got to see patients after they had stopped treatments that were meant to cure the disease. Heck, you can’t get into hospice unless you stop curative treatments. Many expressed similar sentiments as Toby Keith. In medical-speak, “the burdens outweighed the benefits.” There, perhaps, was a time when the benefits were greater, but no more.
Or, to paraphrase Ecclesiastes in the Hebrew Bible, “There is a time for chemo and a time for no chemo.”
Let go and let be.
_____________________
Author Chaplain Hank Dunn, MDiv, has sold over 4 million copies of his books Hard Choices for Loving Peopleand Light in the Shadows (also available on Amazon).






 I read a recent JAMA Online article titled “
I read a recent JAMA Online article titled “ Changing “What does the patient WANT?” to “What does the patient THINK…”
Changing “What does the patient WANT?” to “What does the patient THINK…” Soon after I became a part-time nursing home chaplain in 1983, our administration formed an ethics committee. Virginia had just passed a “Natural Death Act,” which gave patients a right in the code to refuse treatment and provided a form (e.g., “living will”) to express their treatment preferences.
Soon after I became a part-time nursing home chaplain in 1983, our administration formed an ethics committee. Virginia had just passed a “Natural Death Act,” which gave patients a right in the code to refuse treatment and provided a form (e.g., “living will”) to express their treatment preferences. Can we know what God wants? I was drawn to this story reading the pleas for people of faith to pray for a miracle when one could read between the lines and understand that this man was dying.
Can we know what God wants? I was drawn to this story reading the pleas for people of faith to pray for a miracle when one could read between the lines and understand that this man was dying. The family saw this as a sign of God’s intervention. The skeptic might say, “God did not decide the patient should not die during that code. Human intervention went against what seemed to be God’s plan.”
The family saw this as a sign of God’s intervention. The skeptic might say, “God did not decide the patient should not die during that code. Human intervention went against what seemed to be God’s plan.” May 7th, Update! “The doctors are continuing to try and prepare me for the worst. And I continue to explain to them that [we] are people of faith and that our God has the final say. I am not in denial about what’s happening to him or blind to what the medical reports say…. I just know that the God I serve is greater than any infection and more powerful than any organ failure.”
May 7th, Update! “The doctors are continuing to try and prepare me for the worst. And I continue to explain to them that [we] are people of faith and that our God has the final say. I am not in denial about what’s happening to him or blind to what the medical reports say…. I just know that the God I serve is greater than any infection and more powerful than any organ failure.”



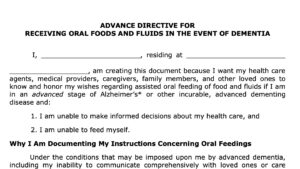
 The patient had left verbal and written instructions that she did not want to have life-saving treatments when she was dying. A “No CPR” order was on her chart. Knowing her daughter’s feelings, the old lady chose her son as her power of attorney. She conspicuously omitted any mention of her daughter in the document.
The patient had left verbal and written instructions that she did not want to have life-saving treatments when she was dying. A “No CPR” order was on her chart. Knowing her daughter’s feelings, the old lady chose her son as her power of attorney. She conspicuously omitted any mention of her daughter in the document. Several years ago, I spoke at the Centra Hospital in Lynchburg, Virginia. There were about 50 people in the room, including members of the clergy, physicians, nurses, social workers, and just plain folks. I divided my presentation, the first half devoted to helping patients and families make end-of-life decisions, and the second half to the emotional and spiritual issues at the end of life.
Several years ago, I spoke at the Centra Hospital in Lynchburg, Virginia. There were about 50 people in the room, including members of the clergy, physicians, nurses, social workers, and just plain folks. I divided my presentation, the first half devoted to helping patients and families make end-of-life decisions, and the second half to the emotional and spiritual issues at the end of life. About six months after the patient died, the lady visited her friend. The now-widow said, “I made a mistake. I made the wrong decision. I should have left the tube out and let him die sooner.”
About six months after the patient died, the lady visited her friend. The now-widow said, “I made a mistake. I made the wrong decision. I should have left the tube out and let him die sooner.” “I know he would never want to be kept alive like this,” she said to me over the sound of a machine forcing air into her husband’s lungs. He lay motionless, eyes closed. He had been like this for months after arriving at the nursing home from the hospital.
“I know he would never want to be kept alive like this,” she said to me over the sound of a machine forcing air into her husband’s lungs. He lay motionless, eyes closed. He had been like this for months after arriving at the nursing home from the hospital. Since she was Jewish and asked this question, I gave her a copy of Rabbi Harold Kushner’s
Since she was Jewish and asked this question, I gave her a copy of Rabbi Harold Kushner’s