Boy, was I blindsided?
 I posted a quote from a study that examined the general public’s understanding of hospice on my Hard Choices for Loving People Facebook page. 30% of the respondents said they felt hospice hastens death. My Facebook post got hundreds of likes and comments, a lot of traffic for my humble page. I had no idea this would engender such a strong response.
I posted a quote from a study that examined the general public’s understanding of hospice on my Hard Choices for Loving People Facebook page. 30% of the respondents said they felt hospice hastens death. My Facebook post got hundreds of likes and comments, a lot of traffic for my humble page. I had no idea this would engender such a strong response.
“This morphine is wonderful”
Misconceptions can be based on misconceptions. When people hear that a friend is receiving morphine, they automatically think death is near. Not necessarily. Because of this close association of morphine with death and the association of getting on morphine in hospice, many assume that’s what hospice does — hastens death. Not so. Morphine controls pain and relaxes breathing.
I had an elderly patient once who was dying of respiratory failure. She was so short of breath that it was a major chore for her to move from her bed to a chair. She got great relief from morphine which she took for months before dying. She told me once, “I’ve always been opposed to drugs, but this morphine is wonderful.”
The coincidence of death after morphine
Many of the respondents to my post who agreed that “hospice hastens death” told stories of family members going on hospice and dying soon after. Why should this surprise us? Hospice requires that a patient is within six months of dying, although the average patient is only on hospice for two weeks.
I am sure it is just a coincidence that a patient receives a dose of morphine and dies shortly after. The family then thinks, “she died because they gave her morphine.” She did not. She was on hospice because she was dying, and she just happened to take her last breath after taking morphine.
No incentive for a hospice to hasten death
 It makes no sense that hospice would want to hasten a patient’s death. The more days the patient is on hospice, the more reimbursement the hospice receives. It is totally against their financial interest to hasten death.
It makes no sense that hospice would want to hasten a patient’s death. The more days the patient is on hospice, the more reimbursement the hospice receives. It is totally against their financial interest to hasten death.
Hospices also want to make sure their patients are as pain-free as possible. Families of hospice patients fill out surveys after the death of their person. They rate the hospice on pain control, among other items.
So, yes, hospices use morphine to keep patients comfortable, not hasten death. They want to have the patient as long as a natural dying process will allow, and they want favorable survey results.
The research is clear; patients live longer on hospice
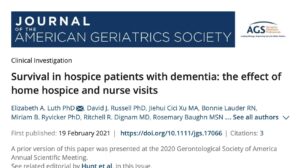
 Many studies confirm that hospice patients live longer than nonhospice patients suffering from the same disease. One study looked at dementia patients. On average, the patients on hospice lived longer than those who never entered a hospice program.
Many studies confirm that hospice patients live longer than nonhospice patients suffering from the same disease. One study looked at dementia patients. On average, the patients on hospice lived longer than those who never entered a hospice program.
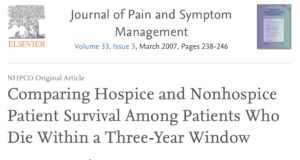
Another study looked at five different kinds of cancer and congestive heart failure. Once again, the patients who were under hospice care lived longer than the nonhospice patients.
So, rest easy. If you have a life-limiting illness and want to live longer with a better quality of life, go into hospice as soon as possible.
________________________________________
Chaplain Hank Dunn is the author of Hard Choices for Loving People: CPR, Feeding Tubes, Palliative Care, Comfort Measures and the Patient with a Serious Illness and Light in the Shadows. Together they have sold over 4 million copies. You can purchase his books at hankdunn.com or on Amazon.


 Rosemary Bowen, at 94, was living independently. She said she had had a wonderful life and did not look forward to a long, slow decline toward death. For years, she had been telling her children, “That her life would not be worth living if she had to depend on caretakers to feed her, dress her, and take her to the toilet.” Then, it happened. She fractured her back and went to rehab but was unable to live independently. That was enough for her.
Rosemary Bowen, at 94, was living independently. She said she had had a wonderful life and did not look forward to a long, slow decline toward death. For years, she had been telling her children, “That her life would not be worth living if she had to depend on caretakers to feed her, dress her, and take her to the toilet.” Then, it happened. She fractured her back and went to rehab but was unable to live independently. That was enough for her. Do not try this without medical support. Rosemary was able to get a hospice to care for her in her last days. Palliative care is also available to ease burdensome symptoms like pain and thirst. See
Do not try this without medical support. Rosemary was able to get a hospice to care for her in her last days. Palliative care is also available to ease burdensome symptoms like pain and thirst. See 


 I have just discovered two great videos with Dr. Michael Greger discussing this very topic. Each video is less than seven minutes and worth every minute of your time. One is called
I have just discovered two great videos with Dr. Michael Greger discussing this very topic. Each video is less than seven minutes and worth every minute of your time. One is called 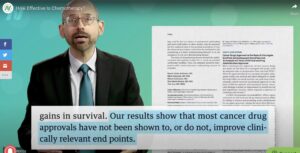 In his second video he referred to a study reported in the Journal of the National Cancer Institute. “In fact, the most expensive drug they looked at, the one costing $169,836 a year, did not improve overall survival at all, and actually worsened quality of life. That’s $169,000 just to make you feel worse with no benefit. Why pay a penny for a treatment that doesn’t actually help?”
In his second video he referred to a study reported in the Journal of the National Cancer Institute. “In fact, the most expensive drug they looked at, the one costing $169,836 a year, did not improve overall survival at all, and actually worsened quality of life. That’s $169,000 just to make you feel worse with no benefit. Why pay a penny for a treatment that doesn’t actually help?” The patient had left verbal and written instructions that she did not want to have life-saving treatments when she was dying. A “No CPR” order was on her chart. Knowing her daughter’s feelings, the old lady chose her son as her power of attorney. She conspicuously omitted any mention of her daughter in the document.
The patient had left verbal and written instructions that she did not want to have life-saving treatments when she was dying. A “No CPR” order was on her chart. Knowing her daughter’s feelings, the old lady chose her son as her power of attorney. She conspicuously omitted any mention of her daughter in the document. How many times have we seen in an obituary, “He died peacefully at home with his family gathered around him.” Families wear this as a badge of honor. They provided the best of care and met the patient’s wishes to remain at home.
How many times have we seen in an obituary, “He died peacefully at home with his family gathered around him.” Families wear this as a badge of honor. They provided the best of care and met the patient’s wishes to remain at home.
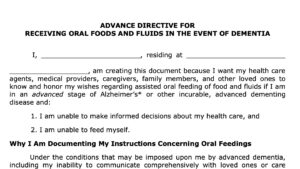
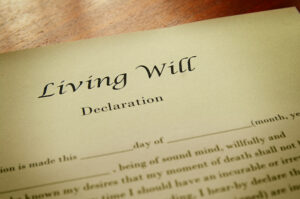 Another change in the last 40 years has been the increased use of advance directive documents like living wills and durable powers of attorney for healthcare. About half the adult population now has such papers.
Another change in the last 40 years has been the increased use of advance directive documents like living wills and durable powers of attorney for healthcare. About half the adult population now has such papers. Several years ago, I spoke at the Centra Hospital in Lynchburg, Virginia. There were about 50 people in the room, including members of the clergy, physicians, nurses, social workers, and just plain folks. I divided my presentation, the first half devoted to helping patients and families make end-of-life decisions, and the second half to the emotional and spiritual issues at the end of life.
Several years ago, I spoke at the Centra Hospital in Lynchburg, Virginia. There were about 50 people in the room, including members of the clergy, physicians, nurses, social workers, and just plain folks. I divided my presentation, the first half devoted to helping patients and families make end-of-life decisions, and the second half to the emotional and spiritual issues at the end of life. About six months after the patient died, the lady visited her friend. The now-widow said, “I made a mistake. I made the wrong decision. I should have left the tube out and let him die sooner.”
About six months after the patient died, the lady visited her friend. The now-widow said, “I made a mistake. I made the wrong decision. I should have left the tube out and let him die sooner.”