Since my bladder cancer diagnosis in May, I have found myself clearing my calendar to allow the next steps in my care to unfold. I am trying to prioritize what I need to do and what can be left undone.

Photo by National Cancer Institute on Unsplash
We met with the doctor last week, reviewed my current situation, and mapped out the next steps in treatment. He is still optimistic that he got all the cancer in the first surgery, even though a second surgery is required to make sure.
Along with the surgery comes weeks of recovery tethered to a catheter and its bag o’ urine. Then, there will be six weekly treatments with more scopes and tests.
In the grand scheme of things, these burdens do not seem too great when I think of patients I have cared for over the years as their hospice chaplain. I am not complaining, nor do I feel life is treating me unfairly. This is all part of life.
Things Left Undone
This newfound status as a cancer patient makes me think of some things that really can be left UNDONE.
I canceled a routine appointment with my optometrist last week. My glasses and “readers” both work fine, even though I occasionally rely on a magnifying glass. I do need to look into having cataract surgery, but that will have to be left UNDONE for now.
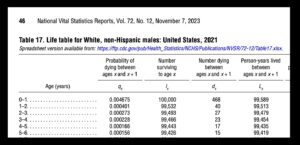 I’ve already had my last colonoscopy a couple of years ago. Even before my cancer, I had accepted the guidelines that there was no need to screen for something that would not kill me before my life expectancy of ten years. And… oh yeah… that was my life expectancy before my cancer diagnosis. A colonoscopy can be left UNDONE.
I’ve already had my last colonoscopy a couple of years ago. Even before my cancer, I had accepted the guidelines that there was no need to screen for something that would not kill me before my life expectancy of ten years. And… oh yeah… that was my life expectancy before my cancer diagnosis. A colonoscopy can be left UNDONE.
As an aside, I found a GeriPal podcast that discusses stopping mammography somewhere between 70 and 75 because there is no benefit for a woman who has no history of breast cancer and who is not expected to live another 10 years.
Things Done
On the other hand, after being diagnosed with bladder cancer, I started a list titled, “Hope for the best, plan for the worst.” I can still work on these items to render them things DONE.
 In the immediate future, I will take a road trip to visit my three children and four grands. I have made this trek two or three times a year for several years. I love driving long distances; this one is over 3,000 miles round trip. I will listen to books and podcasts, see my people, and visit friends, some of them going back to the 1970s. I will also visit places that will bring back so many memories. I want to get this DONE.
In the immediate future, I will take a road trip to visit my three children and four grands. I have made this trek two or three times a year for several years. I love driving long distances; this one is over 3,000 miles round trip. I will listen to books and podcasts, see my people, and visit friends, some of them going back to the 1970s. I will also visit places that will bring back so many memories. I want to get this DONE.
What will I listen to on this trip? The Emperor of All Maladies: A Biography of Cancer by Siddartha Mukherjee. I heard of the 2015 book just this week. I probably would not have been interested in 2015 BC — Before Cancer.
I started a project before Christmas and got stuck. My wife had asked for a bound book of photos chronicling our daughter’s life. I have sorted through hundreds of pictures, but many more remain. This needs to be moved onto the DONE list.
Finally, another kernel of an idea floating in my head is a “life story” in pictures. I wrote a previous blog about the “spiritual autobiography” I gave my family on my 75th birthday last year. So, this would expand the autobiography and incorporate photos I have going back my early days. Get ‘er DONE.
“By what we have done, and by what we have left undone”
These words are familiar to Episcopalians. We recite them every Sunday as part of our confession. It goes, “…we confess that we have sinned against thee in thought, word, and deed, by what we have done, and by what we have left undone.”
Full disclosure: I am more of an “original blessing” guy than “original sin” guy. I give little thought to sin and much appreciation for my blessings. Nonetheless, I borrowed the wording of things “done” and things “left undone” to help me incorporate my cancer diagnosis into the living of these days.
This blog is DONE.
[I explored this same content on a video I posted yesterday on YouTube.]
___________________
Author Chaplain Hank Dunn, MDiv, has sold over 4 million copies of his books Hard Choices for Loving People and Light in the Shadows (also available on Amazon).

 Nothing to Fear: Demystifying Death to Live More by Julie McFadden, RN, is the latest in a long line of books showing the way to a more peaceful and more meaningful dying experience. Why another death and dying book? Why not? Sitting at #8 on the New York Times “Advice” best-seller list, Nothing to Fear is full of advice about navigating the last six months of life under hospice care.
Nothing to Fear: Demystifying Death to Live More by Julie McFadden, RN, is the latest in a long line of books showing the way to a more peaceful and more meaningful dying experience. Why another death and dying book? Why not? Sitting at #8 on the New York Times “Advice” best-seller list, Nothing to Fear is full of advice about navigating the last six months of life under hospice care.
 Throughout Nothing to Fear we see nurse Julie addressing spiritual concerns of her patients and their families. She devotes a whole chapter, “Deathbed Phenomena,” to stories about patients having visions of long dead relatives. Here’s her understanding of these experiences returning to her theme of the metaphor of birth:
Throughout Nothing to Fear we see nurse Julie addressing spiritual concerns of her patients and their families. She devotes a whole chapter, “Deathbed Phenomena,” to stories about patients having visions of long dead relatives. Here’s her understanding of these experiences returning to her theme of the metaphor of birth:


 While waiting for the daughter’s arrival, the ER doc asked me, “What is his code status?” I told him.
While waiting for the daughter’s arrival, the ER doc asked me, “What is his code status?” I told him.

 This story about this patient and his daughter came to mind as I listened to a recent GeriPal podcast,
This story about this patient and his daughter came to mind as I listened to a recent GeriPal podcast, 
 “When I’m dead, I’m dead.… and I just sail off into nothingness, and that brings me a lot of comfort. That doesn’t bring everyone comfort but it brings me comfort.” —Caitlin Doughty, author of
“When I’m dead, I’m dead.… and I just sail off into nothingness, and that brings me a lot of comfort. That doesn’t bring everyone comfort but it brings me comfort.” —Caitlin Doughty, author of 




 To qualify for hospice under the Medicare benefit, a physician has to say, “This patient has, at most, six months to live if the disease runs its normal course.” What happens if the prognosis is wrong and the patient is still alive after six months?
To qualify for hospice under the Medicare benefit, a physician has to say, “This patient has, at most, six months to live if the disease runs its normal course.” What happens if the prognosis is wrong and the patient is still alive after six months?
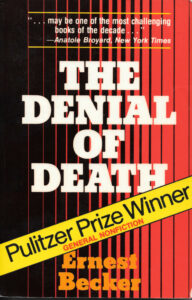 Two months after he died, Ernest Becker won the 1974 Pulitzer Prize for General Nonfiction for his book The Denial of Death. I guess, since he was dead, he was not a winner, but his book was.
Two months after he died, Ernest Becker won the 1974 Pulitzer Prize for General Nonfiction for his book The Denial of Death. I guess, since he was dead, he was not a winner, but his book was.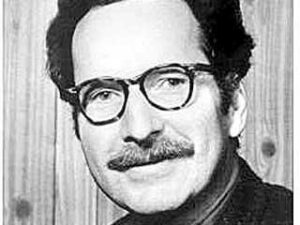 I’ll get to Becker’s deathbed below but first a few quotes from his classic. Note that Becker wrote in 1973 just as we were becoming aware that we no longer refer to all humans as “man.” I know better now but I will let his original words stand.
I’ll get to Becker’s deathbed below but first a few quotes from his classic. Note that Becker wrote in 1973 just as we were becoming aware that we no longer refer to all humans as “man.” I know better now but I will let his original words stand.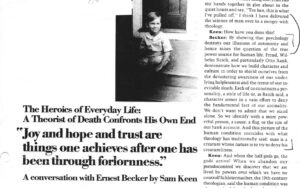 Soon after The Denial of Death arrived in late 1973, Sam Keen, one of the editors at the prestigious Psychology Today magazine, called Becker’s home hoping to set up an interview. Keen explained how the deathbed interview came about: “I called his home in Vancouver to see if he would be willing to tape a conversation. His wife Marie informed me that he had just been taken to the hospital and was in the terminal stage of cancer. The next day she called to say that Ernest would very much like to do the conversation if I could get there while he still had strength and clarity. So I went to Vancouver with speed and trembling, knowing that the only thing more presumptuous than intruding into the private world of the dying would be to refuse the invitation.”
Soon after The Denial of Death arrived in late 1973, Sam Keen, one of the editors at the prestigious Psychology Today magazine, called Becker’s home hoping to set up an interview. Keen explained how the deathbed interview came about: “I called his home in Vancouver to see if he would be willing to tape a conversation. His wife Marie informed me that he had just been taken to the hospital and was in the terminal stage of cancer. The next day she called to say that Ernest would very much like to do the conversation if I could get there while he still had strength and clarity. So I went to Vancouver with speed and trembling, knowing that the only thing more presumptuous than intruding into the private world of the dying would be to refuse the invitation.” When I first walked into the home, I sat alone with the wife in the living room. She was very comfortable talking about her husband’s impending death. I asked her, “What is all this about not wearing our pins or talking about death? Does your husband know he is dying?” She said, “Oh, yes, he knows he is dying.” I asked, “How do you know he knows?” She responded, “Because he asked me.” I asked how she responded to him and she had told him, “Not while I’m around.”
When I first walked into the home, I sat alone with the wife in the living room. She was very comfortable talking about her husband’s impending death. I asked her, “What is all this about not wearing our pins or talking about death? Does your husband know he is dying?” She said, “Oh, yes, he knows he is dying.” I asked, “How do you know he knows?” She responded, “Because he asked me.” I asked how she responded to him and she had told him, “Not while I’m around.”
