Former President Jimmy Carter continues to teach us how to age with grace and meaning. I blogged previously about his going on hospice back in February. Now, six months later, he is still alive and receiving hospice care at home.
Three lessons we can take away from this phase in his life:
-
Hospice care can continue longer than six months
 To qualify for hospice under the Medicare benefit, a physician has to say, “This patient has, at most, six months to live if the disease runs its normal course.” What happens if the prognosis is wrong and the patient is still alive after six months?
To qualify for hospice under the Medicare benefit, a physician has to say, “This patient has, at most, six months to live if the disease runs its normal course.” What happens if the prognosis is wrong and the patient is still alive after six months?
Note the caveat, “if the disease runs its normal course.” Some patients do live longer than is expected. In these cases, the hospice can re-certify that the patient still appears to have six months or less to live.
Some diagnoses are very difficult to guestimate the number of months a patient may have left. For instance, cancers are easier to give a prognosis than dementias. Doctors just do the best they can.
50% of hospice patients are on hospice care for 18 days or less.* 25% receive care for just five days or less. But there are outliers on the long end, with 10% on service for more than nine months. So, Jimmy Carter’s six months does happen more often than you might think.
-
Hospice care is primarily delivered in the place of residence

Carter home in Plains, Georgia. Photo: Library of Congress
Many people think hospice is a place you go to die. Not true. Hospice is a concept of care. 98% of hospice care is delivered in the patient’s residence, whether that is a private home, an assisted living facility, or a nursing home.
A recent Washington Post article gave a window into life in the Carter home now.
“Jimmy Carter is often out of bed first, waiting in his recliner for his wife to emerge. ‘Rosalynn comes in the room and makes a beeline for this chair and bends over and kisses him,’ said Jill Stuckey, a close friend. They spend many hours sitting side by side.”
-
Families usually provide most of the caregiving for hospice patients
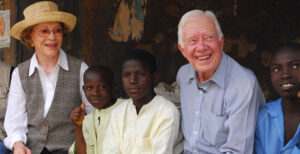
Place: Nasarawa North, Nigeria; Feb. 15, 2007; Credit: The Carter Center
Many families are surprised that hospice does NOT routinely provide round-the-clock care. The family must provide the bulk of the care. Only 1% of hospice dollars go to what is known as “continuous care,” meaning round-the-clock.
Of course, the Carters have the resources to get the best care at home. They have other perks too. The Secret Service gave the couple a ride to watch the Fourth of July fireworks in their hometown.
Interestingly, Rosalyn Carter has had a passion for providing support for family caregivers. When The Carter Center announced that Mrs. Carter was diagnosed with dementia, they commented, “As the founder of the Rosalynn Carter Institute for Caregivers, Mrs. Carter often noted that there are only four kinds of people in this world: those who have been caregivers; those who are currently caregivers, those who will be caregivers, and those who will need caregivers.”
Thank you for your service
The Post asked people who knew them what makes the Carters keep going. “Gerald Rafshoon, who was Carter’s White House spokesman, and others believe a key reason the Carters keep going is that neither wants to leave the other.”
The Carters have lived a life of service and continue to provide an example of how to approach the last days. Thank you, Jimmy and Rosalyn!
_______________
*Statistics in this blog came from the National Hospice and Palliative Care Organization’s “Facts and Figures, 2022 Edition.”
________________________
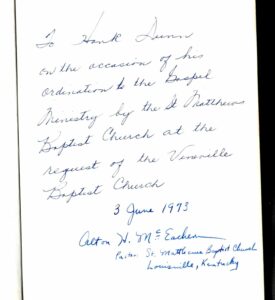
Chaplain Hank Dunn is the author of Hard Choices for Loving People: CPR, Feeding Tubes, Palliative Care, Comfort Measures and the Patient with a Serious Illness and Light in the Shadows. Together they have sold over 4 million copies. You can purchase his books at hankdunn.com or on Amazon.




 I posted a
I posted a  It makes no sense that hospice would want to hasten a patient’s death. The more days the patient is on hospice, the more reimbursement the hospice receives. It is totally against their financial interest to hasten death.
It makes no sense that hospice would want to hasten a patient’s death. The more days the patient is on hospice, the more reimbursement the hospice receives. It is totally against their financial interest to hasten death. Many studies confirm that hospice patients live longer than nonhospice patients suffering from the same disease.
Many studies confirm that hospice patients live longer than nonhospice patients suffering from the same disease.  Rosemary Bowen, at 94, was living independently. She said she had had a wonderful life and did not look forward to a long, slow decline toward death. For years, she had been telling her children, “That her life would not be worth living if she had to depend on caretakers to feed her, dress her, and take her to the toilet.” Then, it happened. She fractured her back and went to rehab but was unable to live independently. That was enough for her.
Rosemary Bowen, at 94, was living independently. She said she had had a wonderful life and did not look forward to a long, slow decline toward death. For years, she had been telling her children, “That her life would not be worth living if she had to depend on caretakers to feed her, dress her, and take her to the toilet.” Then, it happened. She fractured her back and went to rehab but was unable to live independently. That was enough for her. Do not try this without medical support. Rosemary was able to get a hospice to care for her in her last days. Palliative care is also available to ease burdensome symptoms like pain and thirst. See
Do not try this without medical support. Rosemary was able to get a hospice to care for her in her last days. Palliative care is also available to ease burdensome symptoms like pain and thirst. See  How many times have we seen in an obituary, “He died peacefully at home with his family gathered around him.” Families wear this as a badge of honor. They provided the best of care and met the patient’s wishes to remain at home.
How many times have we seen in an obituary, “He died peacefully at home with his family gathered around him.” Families wear this as a badge of honor. They provided the best of care and met the patient’s wishes to remain at home.
 Another change in the last 40 years has been the increased use of advance directive documents like living wills and durable powers of attorney for healthcare. About half the adult population now has such papers.
Another change in the last 40 years has been the increased use of advance directive documents like living wills and durable powers of attorney for healthcare. About half the adult population now has such papers.
 “Charlie” was not a very creative name, but it just seemed to fit a male King Charles Spaniel. At first, we crated him at night. After weeks of barking, he finally settled into his crate and his place at home. Until…
“Charlie” was not a very creative name, but it just seemed to fit a male King Charles Spaniel. At first, we crated him at night. After weeks of barking, he finally settled into his crate and his place at home. Until… Charlie joined Katie in Oxford her second year at Ole Miss, where he supported her during roommate issues and dating cycles. Their deep bond reached new depths. A dog just loves unconditionally.
Charlie joined Katie in Oxford her second year at Ole Miss, where he supported her during roommate issues and dating cycles. Their deep bond reached new depths. A dog just loves unconditionally.

 On Sunday afternoon, my wife and I were pulling into the Walmart parking lot, and she blurted out, “Katie has to come home tonight.” It was a mother’s flash of insight for her soon-to-be grieving daughter. She called Katie and told her to get to National airport and get on a plane. I picked her up in Memphis with Charlie a few hours later. They slept together on our bedroom floor that night before she returned to D.C., Monday. In the car on the way to the Memphis airport, she “Snapped” a photo to friends, “my last photo I’ll ever take with my baby.” Indeed, it was.
On Sunday afternoon, my wife and I were pulling into the Walmart parking lot, and she blurted out, “Katie has to come home tonight.” It was a mother’s flash of insight for her soon-to-be grieving daughter. She called Katie and told her to get to National airport and get on a plane. I picked her up in Memphis with Charlie a few hours later. They slept together on our bedroom floor that night before she returned to D.C., Monday. In the car on the way to the Memphis airport, she “Snapped” a photo to friends, “my last photo I’ll ever take with my baby.” Indeed, it was.
 A
A