Perhaps Hospice Nurse Julie’s book should come with a TRIGGER WARNING: Do not read this book if you do not like the words “Clean, Safe, and Comfortable.” More on that in a minute.
 Nothing to Fear: Demystifying Death to Live More by Julie McFadden, RN, is the latest in a long line of books showing the way to a more peaceful and more meaningful dying experience. Why another death and dying book? Why not? Sitting at #8 on the New York Times “Advice” best-seller list, Nothing to Fear is full of advice about navigating the last six months of life under hospice care.
Nothing to Fear: Demystifying Death to Live More by Julie McFadden, RN, is the latest in a long line of books showing the way to a more peaceful and more meaningful dying experience. Why another death and dying book? Why not? Sitting at #8 on the New York Times “Advice” best-seller list, Nothing to Fear is full of advice about navigating the last six months of life under hospice care.
McFadden is better known as @hospicenursejulie to her followers on Instagram (357K), YouTube (432K) and TikTok (1.5M). An influencer with numbers like that has a ready-made public to drive her book sales. It works the other way too. In a way, her fans helped write the book. She often refers to questions she received from followers or experiences they shared with her. Here’s an example:
“Some people ask me, ‘Why is it so important for people to know that they’re going to die?’ It’s a great question. When people choose to learn about their particular illness and what their death might look like, their fears often are eased as they acknowledge what’s happening. The people who are willing to discuss end-of-life issues and to accept that they’re going to die seem to carry about them a certain type of freedom, and they truly live their last days well. Their fear tends to decrease, and they tend to be freer and more full of life, even though they’re dying.”
I listened to McFadden read the text on Audible my first time through. She comes across as the same nurse Julie we know on social media. I don’t think any actress could have captured the conviction, empathy, and compassion we hear in Julie’s own voice. Typical of me, I liked this book so much I bought it a second time in print form. There were too many quotes I JUST HAD to have.
A Very Practical Book
At bottom, Nothing to Fear is a very practical book — a sort of “how to” guide to a peaceful death on hospice. It is user-friendly with lots of lists with numbers or bullets. Here’s one of my favorites from the “Grief” chapter:
THINGS NOT TO SAY WHEN SOMEONE IS GRIEVING
- “At least she had a long life.”
- “God needed her in heaven more than we needed her here.”
- “Everything works together for good for those who love God.”
- “He’s in a better place.”
- “There’s a reason for everything.”
Three Themes Stand Out
-

@hospicenursejulie
Is the patient “clean, safe, and comfortable”? The answers to this question are always on minds of those on the hospice team. Julie reminds family members to strive to always make sure the patient is clean, safe, and comfortable.
- Dying peacefully can be like the process of childbirth. Nurse Julie is not the first to make this comparison. The hospice movement grew out of the same mindset as the “natural childbirth” revolution in the 1960s. Probably the first book to start us thinking about death positively, Elisabeth Kübler-Ross’s On Death and Dying, came out in 1969. Just like a baby “knows” how to be born, the dying body knows how to die. “Listen to the body” we read often in these pages. Again, from nurse Julie:
“After years as a hospice nurse, I can share this strange but true fact: our bodies are biologically built to die.”
- We need to talk about death and dying for a peaceful death to occur. The quote above about why it is important for people to know they are going to die comes from the chapter titled, “Death Is Not a Dirty Word.” In another chapter titled “Advice for the Dying” we find:
“When you look death in the face, it loses its power to bully you. If your death has not yet been part of the conversation in your family or in your home, then your loved ones may not know it’s okay to talk about it with you. Bring it up first, so they know you’re okay with it, and when you do, don’t sanitize it. Use all the d-words: dying, death, dead, died.”
Spirituality in Nothing to Fear
As a hospice chaplain, I am always on the lookout for how an author handles things spiritual. Nurse Julie seems to be so typical of the scores of hospice nurses I have worked with. It varies widely, but 25% to 75% of hospice patients decline visits from the hospice chaplain. Therefore, often patients and their families get spiritual support from the nurse.
 Throughout Nothing to Fear we see nurse Julie addressing spiritual concerns of her patients and their families. She devotes a whole chapter, “Deathbed Phenomena,” to stories about patients having visions of long dead relatives. Here’s her understanding of these experiences returning to her theme of the metaphor of birth:
Throughout Nothing to Fear we see nurse Julie addressing spiritual concerns of her patients and their families. She devotes a whole chapter, “Deathbed Phenomena,” to stories about patients having visions of long dead relatives. Here’s her understanding of these experiences returning to her theme of the metaphor of birth:
“As much as we’d like to, we simply don’t understand everything about these encounters. They’re mysteries. For my part, I can say that my own few experiences have given me nothing but confidence that a better world awaits us. I do believe that there’s an afterlife because of experiences like these.… In many ways, it feels a lot like the wonder of birth. When I get to see a baby being born, I weep from joy. I look at that baby and wonder, ‘Where did you come from?’ When someone dies, I have that same feeling I get when babies are born. It’s a feeling of home. Of comfort.”
In the chapter titled “What the Dying Process Looks Like,” Julie encourages families to pause just after their person dies and allow this “sacred” moment to sink in. In a section headed, “Death Is Not an Emergency,” we find this:
“Whether you’re with your loved one when they die or you discover that they have died after the fact, there is nothing you have to do immediately. Simply notice that what has happened is sacred. Death is a natural part of life, and you have, in whatever way, participated in your loved one’s journey toward this sacred moment.”
This Book Is Just That Good
I place Nothing to Fear up there with Dr. Ira Byock’s Dying Well (1998), Dr. Atul Gawande’s Being Mortal (2017), and Katy Butler’s The Art of Dying Well (2020). This book is just that good. Nurse Julie combines the powerful bedside stories of Ira Byock and the boatloads of practical advice of Katy Butler.
Even with all these wonderful books, we still see a lot of unnecessary suffering at the end of life. Hopefully by exposing the TikTok generation to a more peaceful way of dying, Nurse Julie can help relieve more of that suffering.
___________________
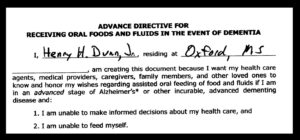
Author Chaplain Hank Dunn, MDiv, has sold over 4 million copies of his books Hard Choices for Loving People and Light in the Shadows (also available on Amazon).
Follow Hank: LinkedIn | Instagram | Facebook | YouTube



 Nothing to Fear: Demystifying Death to Live More by Julie McFadden, RN, is the latest in a long line of books showing the way to a more peaceful and more meaningful dying experience. Why another death and dying book? Why not? Sitting at #8 on the New York Times “Advice” best-seller list, Nothing to Fear is full of advice about navigating the last six months of life under hospice care.
Nothing to Fear: Demystifying Death to Live More by Julie McFadden, RN, is the latest in a long line of books showing the way to a more peaceful and more meaningful dying experience. Why another death and dying book? Why not? Sitting at #8 on the New York Times “Advice” best-seller list, Nothing to Fear is full of advice about navigating the last six months of life under hospice care.
 Throughout Nothing to Fear we see nurse Julie addressing spiritual concerns of her patients and their families. She devotes a whole chapter, “Deathbed Phenomena,” to stories about patients having visions of long dead relatives. Here’s her understanding of these experiences returning to her theme of the metaphor of birth:
Throughout Nothing to Fear we see nurse Julie addressing spiritual concerns of her patients and their families. She devotes a whole chapter, “Deathbed Phenomena,” to stories about patients having visions of long dead relatives. Here’s her understanding of these experiences returning to her theme of the metaphor of birth:

 As the men gather each week, we hand everyone a name badge. Instead of “Hello, My Name is Hank,” each one says simply, “God’s Child.” We all wear one. Incarcerated and free.
As the men gather each week, we hand everyone a name badge. Instead of “Hello, My Name is Hank,” each one says simply, “God’s Child.” We all wear one. Incarcerated and free. When I first walked into the home, I sat alone with the wife in the living room. She was very comfortable talking about her husband’s impending death. I asked her, “What is all this about not wearing our pins or talking about death? Does your husband know he is dying?” She said, “Oh, yes, he knows he is dying.” I asked, “How do you know he knows?” She responded, “Because he asked me.” I asked how she responded to him and she had told him, “Not while I’m around.”
When I first walked into the home, I sat alone with the wife in the living room. She was very comfortable talking about her husband’s impending death. I asked her, “What is all this about not wearing our pins or talking about death? Does your husband know he is dying?” She said, “Oh, yes, he knows he is dying.” I asked, “How do you know he knows?” She responded, “Because he asked me.” I asked how she responded to him and she had told him, “Not while I’m around.”
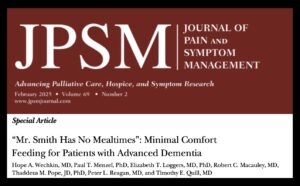
 I read a recent JAMA Online article titled “
I read a recent JAMA Online article titled “ Changing “What does the patient WANT?” to “What does the patient THINK…”
Changing “What does the patient WANT?” to “What does the patient THINK…” Soon after I became a part-time nursing home chaplain in 1983, our administration formed an ethics committee. Virginia had just passed a “Natural Death Act,” which gave patients a right in the code to refuse treatment and provided a form (e.g., “living will”) to express their treatment preferences.
Soon after I became a part-time nursing home chaplain in 1983, our administration formed an ethics committee. Virginia had just passed a “Natural Death Act,” which gave patients a right in the code to refuse treatment and provided a form (e.g., “living will”) to express their treatment preferences.
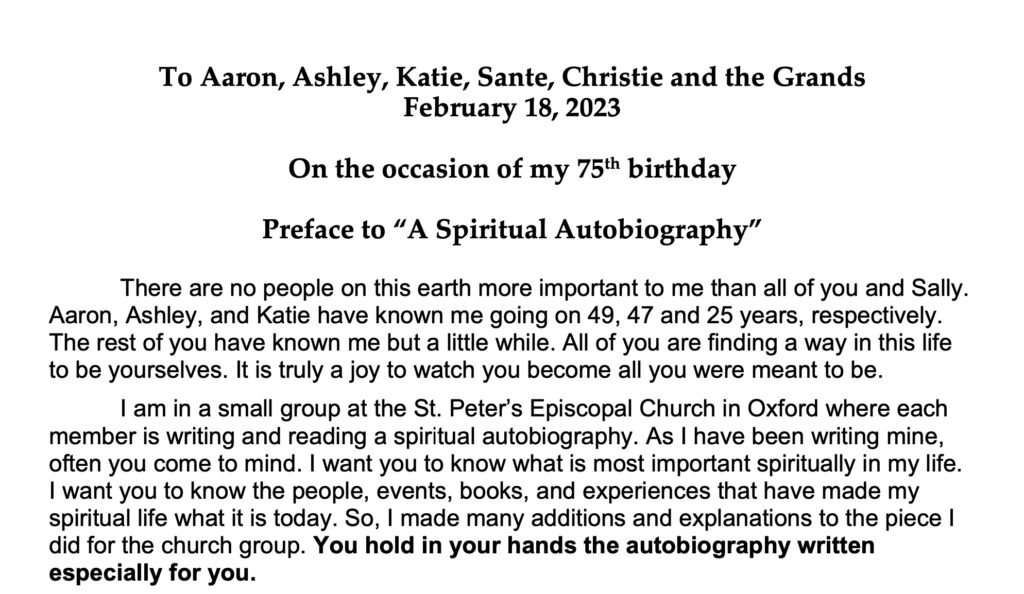
 I have no control over whether anyone cares about what makes me tick. I cast these words out into the sea of my legacy, perhaps to drift on as flotsam. It’s what I can do in these last years of my life. Well, hopefully years.
I have no control over whether anyone cares about what makes me tick. I cast these words out into the sea of my legacy, perhaps to drift on as flotsam. It’s what I can do in these last years of my life. Well, hopefully years. I was such a scaredy-cat at 8 years old. All I can remember of two particular movies in 1956 was that I kept my eyes closed during the entirety of each film. I have just discovered, through Wikipedia, that
I was such a scaredy-cat at 8 years old. All I can remember of two particular movies in 1956 was that I kept my eyes closed during the entirety of each film. I have just discovered, through Wikipedia, that  I just placed the latest “deep field” photo from the new James Webb Space Telescope to my home screen on my iPhone. This is a time exposure photo of a portion of the night sky the size of a grain of sand held at arms-length. Thousands of galaxies appear as we look back billions of years. Each galaxy has billions of stars — each star is not unlike our sun.
I just placed the latest “deep field” photo from the new James Webb Space Telescope to my home screen on my iPhone. This is a time exposure photo of a portion of the night sky the size of a grain of sand held at arms-length. Thousands of galaxies appear as we look back billions of years. Each galaxy has billions of stars — each star is not unlike our sun. How many times have we seen in an obituary, “He died peacefully at home with his family gathered around him.” Families wear this as a badge of honor. They provided the best of care and met the patient’s wishes to remain at home.
How many times have we seen in an obituary, “He died peacefully at home with his family gathered around him.” Families wear this as a badge of honor. They provided the best of care and met the patient’s wishes to remain at home.