In early March, I noticed blood in my urine. “That’s curious,” I thought. It happened twice in one week, so I went to urgent care. They ran a urinalysis and confirmed, “Yep. You have blood in your urine.” The PA went on to list the possibilities of what could cause this: kidney stones, prostate problems, bladder cancer, or it could be nothing.
I told her my father was treated successfully for bladder cancer at about my age (76), and my brother died from it at age 64. Her first response when I told her about my brother’s early death was, “I’m so sorry.” I took it to mean she was sorry about me losing my brother. That moment of empathy has meant so much to me. She could have gotten all clinical on me, saying bladder cancer does run in families. But she first said, “I’m so sorry.”
I have entered the land of cancer patients.

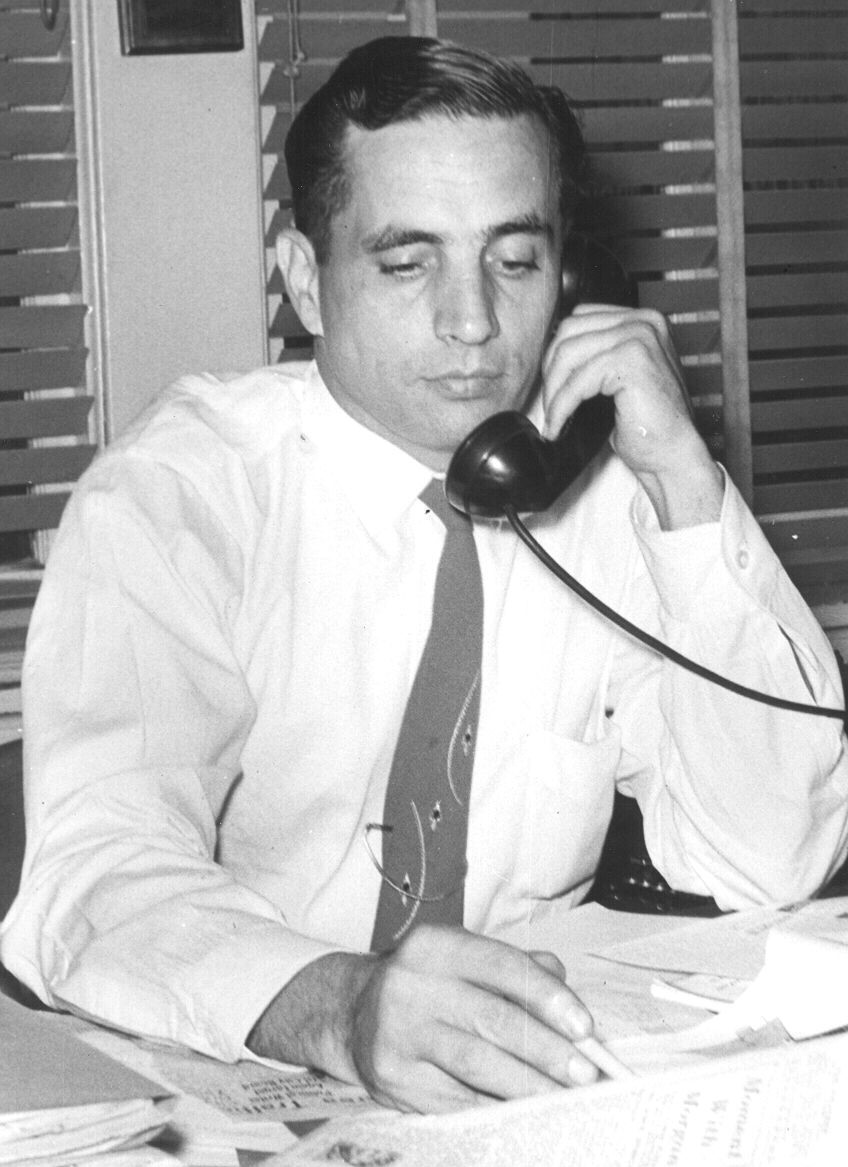
Visiting my father at the nursing home three years before he died
By the time my father got bladder cancer he was already diagnosed with Parkinson’s and had had a couple of small strokes. He had mobility problems and depended on Mom for much of his daily care. His mind was still sharp, and he continued to write professionally, dictating a history column to Mom each week. He couldn’t type anymore. His cancer was removed from the bladder with surgery followed by flushing with medications. As far as we knew, he never had another problem with it.
But his other conditions forced him into a nursing home at age 81, and he finally died soon after his 85thbirthday. He was demented, incontinent of bowel and bladder, unable to recognize family or interact meaningfully to the world around him.
At the time of his bladder cancer diagnosis, we never discussed the possibility of NOT treating it, given that it was caught early, and the treatment was not burdensome. But surviving cancer allowed his slow decline of nine years toward a merciful death. I am sure, if my father were asked, he would have absolutely wanted to treat the cancer. Even if he could have been told about what his next nine years would look like, I think he would want to be cured of cancer.

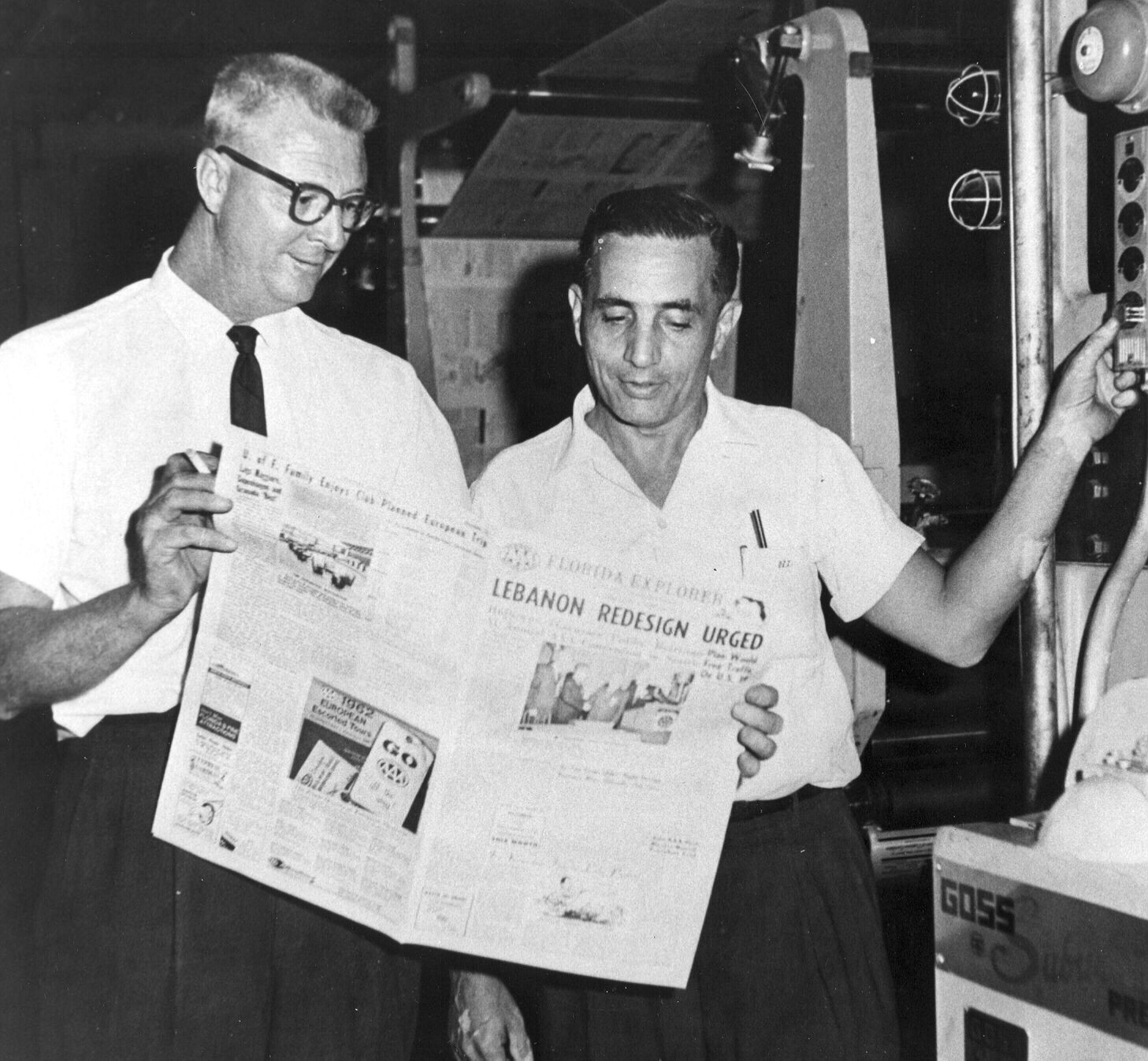
My brother, Dennis, at a horseshoeing competition
My brother’s bladder cancer was quite advanced when he was diagnosed. He did seek a cure, but the cancer continued to spread, and he was gone ten months after blood showed up in his urine. Three years ago, I wrote a previous blog where I mentioned Dennis’ death.
Dennis was a robust 63-year-old when diagnosed. He was a farrier by profession, a demanding job shoeing horses. He was constantly inhaling fumes from the forge which probably led to his death. Smoking and exposure to smoke are risk factors that can lead to bladder cancer. My dad was a heavy smoker for half of his adult life.
And me?

Hank (left) and his sister Janice with their brother Dennis two weeks before he died
I’ve joined a group I did not choose. At this point I do not know if I will be my father or my brother. That is, a journey of 9 years from my dad’s diagnosis of cancer to his death by other killers at age 85 or a 10-month, painful journey my brother took from diagnosis to death. Of course, I won’t be Dennis in that I am already 12 years past the age he died.
I am guessing I am like other newly-diagnosed cancer patients, and I entertain the possibility that I could die sooner rather than later. Going to that place does not make me sad — at least, it doesn’t today. According to the National Vital Statistics Reports, 44% of White males born in the U.S. in my birth year, 1948, have already died. We are just two years away from it being 50%. If my end comes in two years, I would be just average.
No reason to begrudge living an “average” lifespan. As a matter of fact, I should be thankful since half my cohort will have already died.
Grateful indeed!
___________________
Author Chaplain Hank Dunn, MDiv, has sold over 4 million copies of his books Hard Choices for Loving People and Light in the Shadows (also available on Amazon).
Follow Hank: LinkedIn | Instagram | Facebook | YouTube