I have entered a medical-screening twilight zone. When I was in my 60s, I always got colon and prostate cancer screenings. Now, at 74, I am thinking about stopping the screenings.

Photo by Hush Naidoo Jade Photography on Unsplash
JAMA Internal Medicine recently published a research letter — “Comparison of US Cancer Center Recommendations for Prostate Cancer Screening With Evidence-Based Guidelines.” The guidelines recommend that all men 50–70 years old have an annual screening, regardless of their risk factors for prostate cancer. They suggest the patient and clinician share the decision to do this screening.
The clinician should also inform the patient of both the risks and benefits of the screening. There are downsides to prostate cancer screenings at any age — false positives, misdiagnoses, and overtreatment. Treatment can cause urinary, bowel, or sexual function problems — things I would rather avoid.
Why stop at 70? Turns out, the research shows that annual screenings of men with no other risk factors for prostate cancer do NOT reduce their chance of dying of all causes. In other words, both men who did and did not get screened lived about the same number of years.
My greatest fear is dementia
My greatest fear is that I spend my last years with Alzheimer’s, fully demented and a great burden to my family. Once I get that diagnosis, I would welcome an earlier death by cancer.
Years ago, I heard the story of a woman in a nursing home who no longer recognized her family because of dementia, and she had a mastectomy. They saved her life so she could get more demented.
I did not know this woman and her family well enough to hear about their decision-making process. Perhaps, the patient had stated before losing her mind that she wanted everything done to keep her alive. Maybe, her physicians told the family they had to do the surgery and gave them little choice.
I do not judge this family and their decisions. I take it as a warning for my family and me.
In my case, let the cancer grow
If I live to my 90s but am confined to a wheelchair in a memory-care unit, I do NOT want to be checked for cancer. We do not allow euthanasia in this country, but we do respect a patient’s right to refuse treatment. For me, in the presence of dementia, I would want cancer to run its course. Perhaps this could save my family years of heartaches.
__________________________________________
Chaplain Hank Dunn is the author of Hard Choices for Loving People: CPR, Feeding Tubes, Palliative Care, Comfort Measures and the Patient with a Serious Illness and Light in the Shadows. Together they have sold over 4 million copies. You can purchase his books at hankdunn.com or on Amazon.


 “Charlie” was not a very creative name, but it just seemed to fit a male King Charles Spaniel. At first, we crated him at night. After weeks of barking, he finally settled into his crate and his place at home. Until…
“Charlie” was not a very creative name, but it just seemed to fit a male King Charles Spaniel. At first, we crated him at night. After weeks of barking, he finally settled into his crate and his place at home. Until… Charlie joined Katie in Oxford her second year at Ole Miss, where he supported her during roommate issues and dating cycles. Their deep bond reached new depths. A dog just loves unconditionally.
Charlie joined Katie in Oxford her second year at Ole Miss, where he supported her during roommate issues and dating cycles. Their deep bond reached new depths. A dog just loves unconditionally.

 On Sunday afternoon, my wife and I were pulling into the Walmart parking lot, and she blurted out, “Katie has to come home tonight.” It was a mother’s flash of insight for her soon-to-be grieving daughter. She called Katie and told her to get to National airport and get on a plane. I picked her up in Memphis with Charlie a few hours later. They slept together on our bedroom floor that night before she returned to D.C., Monday. In the car on the way to the Memphis airport, she “Snapped” a photo to friends, “my last photo I’ll ever take with my baby.” Indeed, it was.
On Sunday afternoon, my wife and I were pulling into the Walmart parking lot, and she blurted out, “Katie has to come home tonight.” It was a mother’s flash of insight for her soon-to-be grieving daughter. She called Katie and told her to get to National airport and get on a plane. I picked her up in Memphis with Charlie a few hours later. They slept together on our bedroom floor that night before she returned to D.C., Monday. In the car on the way to the Memphis airport, she “Snapped” a photo to friends, “my last photo I’ll ever take with my baby.” Indeed, it was.


 About that same time, I started traveling around the country making presentations to healthcare professionals. My most popular talk, “Helping Patients and Families with End-of-Life Decisions,” includes a series of slides with “Hank’s Theorems” on various end-of-life issues. The first slide says, “The peacefulness of a death is directly proportional to the distance from the hospital ICU.”
About that same time, I started traveling around the country making presentations to healthcare professionals. My most popular talk, “Helping Patients and Families with End-of-Life Decisions,” includes a series of slides with “Hank’s Theorems” on various end-of-life issues. The first slide says, “The peacefulness of a death is directly proportional to the distance from the hospital ICU.”

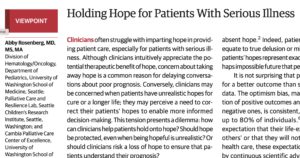 The Journal of the American Medical Association recently published an opinion piece,
The Journal of the American Medical Association recently published an opinion piece,