Julie McFadden was just interview by “Hospice News.” That would be HospiceNurseJulie to her 347K followers in Instagram, 1.5M followers on TikTok, and 420K subscribers on YouTube. AND she just taped a show with Dr. Phil.

Photo-courtesy-of-Julie-McFadden
Julie also has a book coming out in June, Nothing to Fear: Demystifying Death to Live More Fully.
It’s a great short interview. Here are some excerpts:
Reflecting on her work as an ICU nurse, she said, “We think [death is] the worst possible thing that could happen, and I think that causes a lot of undue suffering. And suffering to me is far worse than death.”
“I do feel like it was kind of traumatic to be an ICU nurse, at least for me. Hospice was a slower pace. I was in people’s homes. There was a lot of autonomy.”
“Even as an experienced ICU nurse, I feel like I didn’t understand the scope of how our bodies really take care of us, even at the end of life.”
[The interviewer asked] “Can you expound on that a little bit? What are some of the ways that our bodies take care of us?”
“For example, almost everyone wasn’t hungry, wasn’t eating and drinking, and they were sleeping a lot of the time.…. When you start getting towards the end of life, your body knows it. So it starts like turning off that hunger and thirst mechanism in the brain, because it knows that it doesn’t really need that anymore.”
Read it for yourself. Check it out at “Hospice News.”
_____________________
Author Chaplain Hank Dunn, MDiv, has sold over 4 million copies of his books Hard Choices for Loving People and Light in the Shadows (also available on Amazon).
Follow Hank: LinkedIn | Instagram | Facebook | YouTube



 I am guessing if, during that last phone call, Favre asked, “Do you regret getting the chemo?” Keith might have responded, “Not at all.” Perhaps it bought him some time. Maybe, earlier in the treatment, he did not think it was causing “more damage… than the cancer.”
I am guessing if, during that last phone call, Favre asked, “Do you regret getting the chemo?” Keith might have responded, “Not at all.” Perhaps it bought him some time. Maybe, earlier in the treatment, he did not think it was causing “more damage… than the cancer.”

 I posted a
I posted a  It makes no sense that hospice would want to hasten a patient’s death. The more days the patient is on hospice, the more reimbursement the hospice receives. It is totally against their financial interest to hasten death.
It makes no sense that hospice would want to hasten a patient’s death. The more days the patient is on hospice, the more reimbursement the hospice receives. It is totally against their financial interest to hasten death. Many studies confirm that hospice patients live longer than nonhospice patients suffering from the same disease.
Many studies confirm that hospice patients live longer than nonhospice patients suffering from the same disease.  How many times have we seen in an obituary, “He died peacefully at home with his family gathered around him.” Families wear this as a badge of honor. They provided the best of care and met the patient’s wishes to remain at home.
How many times have we seen in an obituary, “He died peacefully at home with his family gathered around him.” Families wear this as a badge of honor. They provided the best of care and met the patient’s wishes to remain at home.
 Another change in the last 40 years has been the increased use of advance directive documents like living wills and durable powers of attorney for healthcare. About half the adult population now has such papers.
Another change in the last 40 years has been the increased use of advance directive documents like living wills and durable powers of attorney for healthcare. About half the adult population now has such papers. Recently,
Recently,  Then, of course, “happy” is
Then, of course, “happy” is 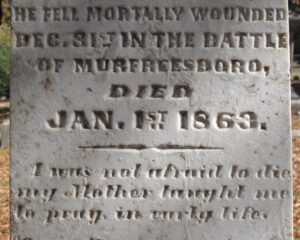 Recently, I
Recently, I